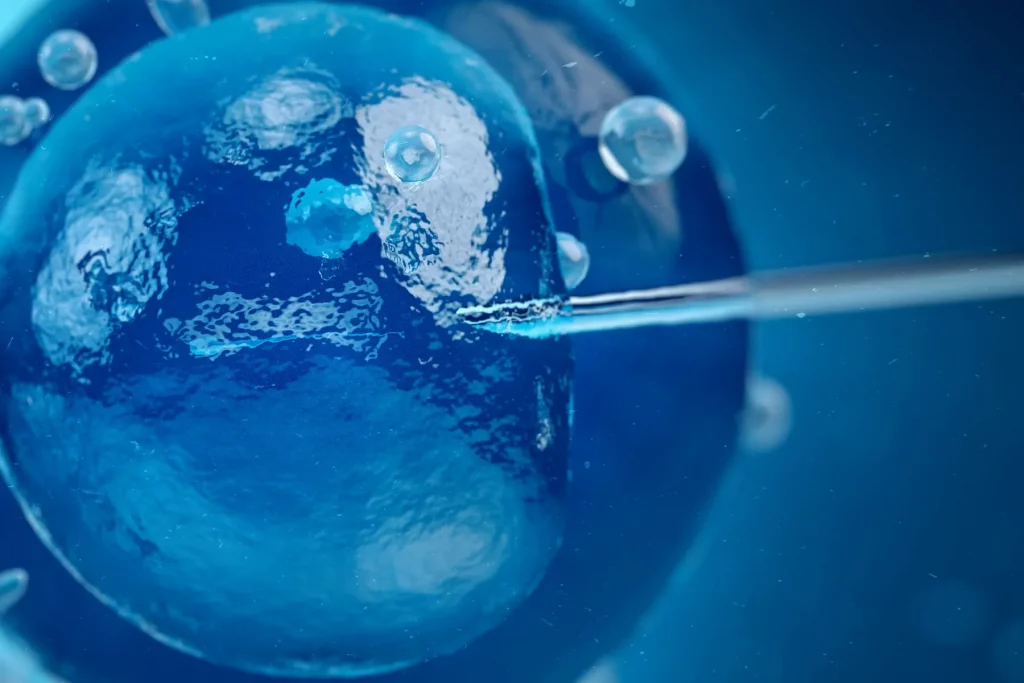
Feb. 9, 2023 — Planning to start or expand your family by 2033? Thanks to emerging technologies in the field of in vitro fertilization, conceiving a baby in this near future might look like something out of a science fiction movie more so than it does today.
Artificial intelligence already plays a role in the complex laboratory process, and its uses are likely to grow. Precision 3D printing and advanced microscopes also have the potential to help identify embryos more likely to result in a healthy pregnancy.
“I can’t believe how far we’ve come in the four decades I’ve been doing this,” says David Gardner, PhD, scientific director at Melbourne IVF in East Melbourne, Victoria, Australia. “But what I’m really excited about [is] where the next 5 to 10 years are going. I feel we’re on the verge of something monumental.”
Here’s a glimpse of tomorrow’s IVF tech.
An Assist for Embryo ‘Artisans’
Deciding which embryo to implant in a patient’s womb is like judging a beauty contest, says Denny Sakkas, PhD, scientific director at Boston IVF in Waltham, MA, who with Gardner published a paper on the future of IVF in the journal Fertility and Sterility.
An experienced embryologist can pick out a good-looking one at a glance. Could AI do the same — in less time and for less money?
“You can teach, mathematically using AI, software to look at features of an embryo that led to a pregnancy versus one that did not,” Sakkas says. He likens the technology to the facial recognition feature on a smartphone: “We’re hoping to do that with images or videos of embryos.”
Even two embryologists in the same lab may grade the same embryo differently. How do you train a machine to perform a subjective task?
Current algorithms use just a bit of the data collected from a time-lapse incubator — a gadget that takes real-time images of an embryo’s development — failing to paint a full picture of its health.
As scientists study how well AI can compete with embryologists, Gardner and Sakkas argue that the combination of human and machine intelligence in embryo selection could be the key to not only maximizing successful pregnancies but also reducing the time it takes people struggling with infertility to conceive.
Automating even part of the process may help alleviate the projected shortage of embryologists, who Gardner calls “artisans,” as demand for IVF increases. IVF is a type of assisted reproductive technology, or ART. More than 83,900 babies conceived via ART were born in the United States in 2019, according to the CDC. That’s up from about 60,200 in 2009. In a previous paper in the journal Reproductive BioMedicine Online, Gardner asked, “Where are all the highly trained embryologists and physicians required for this growth going to come from?”
Another goal of automation is to make IVF cheaper and more geographically accessible to prospective parents. In the United States, a single cycle of IVF costs an average of $10,000-$15,000, according to the Society for Assisted Reproductive Technology. Only 14 states require insurance to cover at least part of the procedure — meaning many people must pay out of pocket. As of 2013, about 40% of reproductive-age women nationwide — more than 25 million — lived in areas with limited or no access to ART clinics.
IVF is a physically and emotionally draining journey even without these barriers, Sakkas says.
“Our research is more aimed at making that experience easier,” he says. “Currently, it’s a very small percentage of infertility couples that actually get treated.”
From 2015 to 2019, roughly 13% of women ages 15-49 had difficulty getting pregnant or carrying a baby to term, according to the CDC’s National Survey of Family Growth. Fewer than 1% had ever received ART treatment.
Still, with machine learning comes a host of other issues, says Aaron Levine, PhD, a bioethicist and associate dean for research and outreach at Georgia Tech’s Ivan Allen College of Liberal Arts, in Atlanta. The technology is only as decent as the humans behind it.
“People developing AI for IVF need to be cognizant of ensuring their algorithms are trained on and work for patients from a wide variety of backgrounds,” Levine says. “We know, for instance, in the U.S. context, that Black and Hispanic patients tend to have worse access to IVF care and worse outcomes when they are able to access this care. It would be very unfortunate if integrating AI into IVF practices exacerbated these already problematic disparities.”
Fabricated Fallopian Tubes and ‘Egg Cups’
Reproductive medicine has come a long way since Louise Brown, the world’s first “test tube baby,” was born in England in 1978. But some things haven’t changed.
“We grow the embryos in a polystyrene dish — just as a tissue culture is done — and they sit in a drop of medium,” Gardner says. “It’s a static system; nothing happens. The embryo sits there and grows, and that’s been the way for 40-odd years.”
By contrast, a naturally conceived embryo is always on the move, exchanging biochemical signals with its parent as it travels from a fallopian tube to the uterus.
Enter microfluidics and 3D printing. Researchers have tested devices small enough to hold a single embryo, Gardner says, which is about the size of a pinhead.
“Rather than having an embryo sitting in a micro-drop, we can now put it into a ‘nest,’” he says. “Then we can pass continuous environments over it and take messages from it, so it becomes a more interactive culture — just like it would be inside mom.”
Micro-fabrication also has implications for sperm and unfertilized eggs.
Scientists in Canada and Australia experimented with such a device designed to mimic the thousands of tissue folds inside the fallopian tubes, which guide sperm to an egg. The device allowed researchers to not only select high-quality sperm, but also do so three times as quickly as the traditional method, according to a 2021 study in the journal Lab on a Chip.
Gardner expects similar technology will absorb needle stress when a single sperm is inserted into an egg in a process called intracytoplasmic sperm injection, or ICSI.
“ICSI is very invasive; we’re developing chambers to basically act as an egg cup to hold the egg safer,” Gardner says. Such 3D-printed tools “aren’t available clinically — this is about the future.”
Younger couples without known fertility problems may one day take advantage of these technologies, too, Gardner and Sakkas wrote, with the goal of freezing the healthiest possible embryos for later use.
The Future Is (Nearly) Now
Despite the promise of these and still other IVF innovations — including sophisticated microscopes that could help shed light on an embryo’s metabolic health — roadblocks remain.
“It’s a very arduous path,” Sakkas says. “Not all technologies reach fruition.”
For starters, IVF doesn’t attract as much funding as other areas of medical research. Last year, the National Institutes of Health funded an estimated $7.6 billion in cancer research, compared to $618 million toward contraception and reproduction study.
Jennifer Kawwass, MD, medical director at the Emory Reproductive Center in Atlanta, is optimistic about the long-term uses of AI for everything from follicle measurement to trigger shot timing. To date, though, relevant studies haven’t shown a definitive advantage over existing practices, she says.
“There is a fine balance between adopting new technology quickly and introducing it before it has proven benefit,” Kawwass says. “Continued innovation, with guarded adoption as its benefit is proven, certainly has a role in the fertility field in the coming years.”
Gardner, too, is tempering his excitement with patience.
“Automation is going to come,” he says. “But I think that’s going to be probably 5 to 10 years away.”